STPs
What are STPs?
STP stands for Sustainability and Transformation Partnership. In December 2015, NHS England announced that health and care organisations, grouped into 44 regional ‘footprints’, would be tasked with developing local plans - called Sustainability and Transformation Plans - to deliver the Five Year Forward View (5YFV) and show how local services will evolve and become sustainable over the next five years.
The 44 footprints published their plans before January 2017 with the aim of addressing three key gaps set by the 5YFV:
- The health and wellbeing gap
- The care and quality gap
- The funding and efficiency gap
The plans are now going through a process of public and clinical engagement and will be subject to further changes.
In the 2017 Spring Budget the government announced that the strongest STPs will receive £325m of capital funding spread over three years. Further funding is expected to be announced in the Autumn Budget as a multi-year capital programme to support the implementation of approved high quality plans.
Which one is my local STP and what does it say?
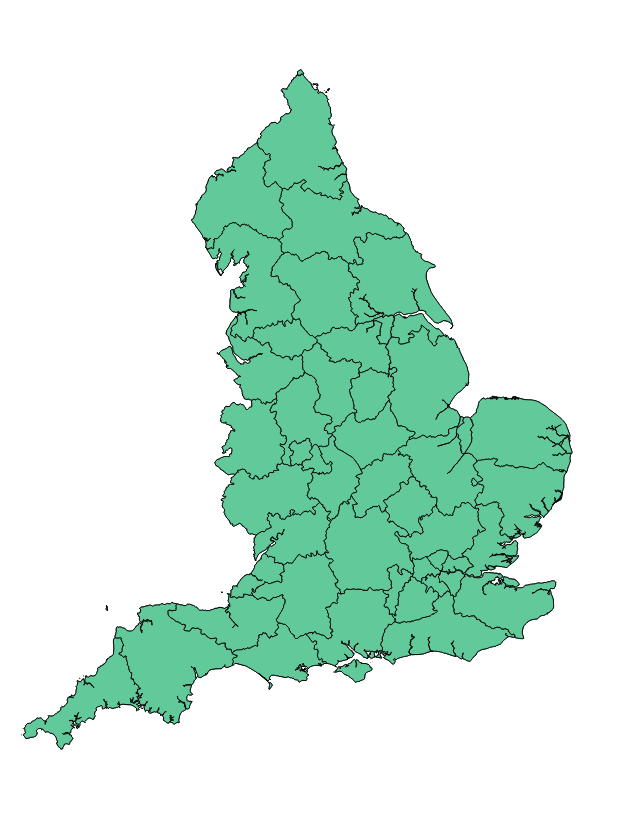
Click on the STP regional footprints below for more information.
What is the possible impact on my work?
Five key issues that are likely to affect surgery
1. Reconfiguration of acute services
Most STPs are considering options to reconfigure acute services. A number of plans are proposing centralising or consolidating specialised services, most commonly orthopaedics, neurosurgery, maternity and paediatrics. Some plans are also considering reducing the number of acute sites and community hospitals through mergers, closing hospital beds and downgrading A&E departments. The RCS is concerned that some proposals plan to reduce beds to an unsustainable level although NHS England has recently introduced a “beds test” to ensure any reduction is achievable without causing problems for patient care such as through creating more out-of-hospital support.
2. Split between emergency and planned care
NHS England is encouraging STPs to look for opportunities to split emergency and urgent care beds or facilities to allow more efficient use of beds for planned surgery, and avoid the risk of cancelled operations due to emergency admissions.
3. Optimising elective care pathways
Some plans are proposing to optimise elective pathways with the aim of reducing variation in the delivery of planned care. Some examples of the proposals to improve elective pathways include reducing the number of unnecessary outpatient appointments, optimising the use of staff and theatres and ensuring timely discharge planning.
4. Rationing
Some plans suggest that CCGs might review funding thresholds for procedures of limited clinical value, such as cataract surgery and hip and knee replacements.
5. Workforce
Some of the workforce proposals are aimed at providing staff with a skills mix to deliver the new models of care across organisation boundaries and services. This includes the use of Multi-Disciplinary Teams and the creation of new roles, such as physician associates, general practice pharmacists and advanced clinical practitioners. However, concerns have been raised about reductions in workforce numbers, not only for staff employed in administrative functions, but also for nurses and GPs. This has led to NHS Improvement establishing a taskforce, made up of senior figures from arm’s length bodies, set up to examine and challenge the STPs’ workforce proposals.
What do the footprints look like?
In order to develop local plans, the whole of England has been divided into 44 geographical areas grouping health and care organisations. On average, each footprint covers a population of 1.2 million people and counts approximately five Clinical Commissioning Groups (CCGs) and seven NHS Trusts – with variation across different regions.
STP footprints
| Average | Minimum | Maximum | |
|---|---|---|---|
| Population | 1.2m | 300,000 | 2.8m |
| CCGs | 4.8 | 1 | 12 |
| Local authorities | 5.8 | 1 | 20 |
| Trusts | 6.7 | 2 | 18 |
Local footprints were created using a number of factors, including geography, scale, existing programmes and relationships, the financial sustainability of organisations in an area, the leadership capacity and the capability to support change. However, the NHS England’s Next Steps On The Five Year Forward View, which was published in March 2017, made it clear that STPs will be able to propose adjustments to their geographical boundaries when appropriate.
Who is in charge?
A number of health and care organisations are members of their local STPs, including CCGs, Local Authorities and NHS Trusts. The structure of governance varies across STPs. However, so far the parternships have not had the powers of a legal entity and STP leads were initially appointed by NHS England for each footprint.
More recently, the update on the Five Year Forward View published last March proposed new governance. For example, all STPs will be able to form a board, establish decision-making mechanisms or reappoint an STP lead through a fair process.
The RCS and STPs
Want to know more about your local STP? Contact us
If you have any questions about your STP or would like to be put in touch with your RCS regional team, please email us at publicaffairs@rcseng.ac.uk
Is there any more STP information available from the RCS?
- Read the RCS President Clare Marx's blog on STPs from October 2016: Give Sustainability and Transformation Plans a Chance
- Read The Bulletin article from March 2017: STPs: the story so far
What is the RCS doing?
The RCS is continuing to monitor the progress of STPs across England. We will champion positive proposals, but also challenge plans which might harm surgical care. We are also encouraging members to contact us about their local plans, so please do get in touch.
I want to know more - what else can I read?
Below are a few sources you might find useful to read.
NHS England
The King's Fund
- STPs explained
- Sustainability and Transformation Plans in the NHS
- Delivering Sustainability and Transformation Plans
