Guidance for surgeons working during the COVID-19 pandemic

Published: 12pm, 20 March 2020
Note: Accompanying guidance was issued on 26 March 2020.
This text is taken from a document approved jointly by the Surgical Royal Colleges of the UK and Ireland, and hosted here for the convenience of mobile users. Download the original statement here.
1. Introduction
1.1 The surgical workforce will need to adapt during the COVID-19 pandemic.
1.2 Priorities in list of importance are:
i) Maintain emergency surgery capabilities
ii) Protect and preserve the surgical workforce
iii) Fulfil alternate surgical roles
iv) Fulfil alternate non-surgical roles
1.3 Surgical workforces are likely to be depleted as clinicians self-isolate. Maintaining normal surgical sub-specialty emergency services will be increasingly difficult.
1.4 Surgical theatre capacity is likely to decrease. Surgeons are likely to be redeployed to support non-surgical specialties.
1.5 The General Medical Council has already indicated its support for this in the exceptional circumstances we are likely to face: gmc-uk.org/news/news-archive/how-we-will-continue-to-regulate-in-light-of-novel-coronavirus.
1.6 The overarching principles are:
i) To triage and deliver healthcare to patients for maximal benefit as in a mass casualty scenario
ii) To protect and preserve the surgical workforce
1.7 Any plans must be dynamic, reactive and will change as the situation/scale unfolds. Surgeons will need to be flexible, collaborative and show leadership in what are expected to be testing times.

2. Priority 1: Maintain emergency surgery capabilities
2.1 The key aim of the surgical workforce is to maintain emergency surgery provision, including major trauma.
2.2 Initially, this will be delivered by individual specialty rotas. These will include rotas where some members of the team do not come into work and act as a healthy reserve.
2.3 If the workforce is reduced due to sickness, individual specialty rotas may no longer be sustainable. In that scenario it may be necessary to move to a generic surgeon rota. This would be based around competencies and would manage the initial triage, some of the surgery and the post-operative management.
2.4 It is likely that the workforce will break down into torso/cavity surgeons (vascular, general, urology) and extremity surgeons (orthopaedics, plastics). Virtual support from specialists would be required for the generic surgeon. Some of the operations will still require a specialist surgeon when available.
2.5 It is suggested that each site would have the presence of a torso surgeon and an extremity surgeon with middle grades. The shift pattern would be 24hrs or 12hrs depending on numbers of surgeons and tempo.
2.6 Major trauma (MT) pathway has been identified as a national priority. Surgeons may be required to take over running the MT service, including trauma team leader (TTL) role, depending on local arrangements.
2.7 Regional solutions may be required if smaller surgical units collapse. The existing Major Trauma Networks are likely to be the best vehicle to achieve this.
3. Priority 2: Protect and preserve the surgical workforce
3.1 It is vital that risk to staff is minimised. This can be achieved by:
i) Non-surgical solutions to be used to avoid surgery where possible
ii) Personal protective equipment (PPE) used correctly in line with national guidance
iii) Rest and recuperation factored in to all planning
iv) Psychological support factored in to all planning
4. Priority 3: Fulfil alternate surgical roles
4.1 Due to the pressure on Emergency Departments, non-respiratory emergencies may be triaged to an alternate pathway which may need support from surgeons (Non-COVID ED). This could be incorporated into providing TTL cover for Major Trauma Centres/Trauma Units, depending on existing local arrangements.
5. Priority 4: Fulfil alternate non-surgical roles
5.1 If all other priorities have been met and the surgical workforce has been maintained, it may be possible for some surgeons to take on non-surgical roles.
5.2 These could include running level 2/3 units or non-clinical roles in command & control. Individuals will need training/mentoring/support in these roles outside their normal practice.
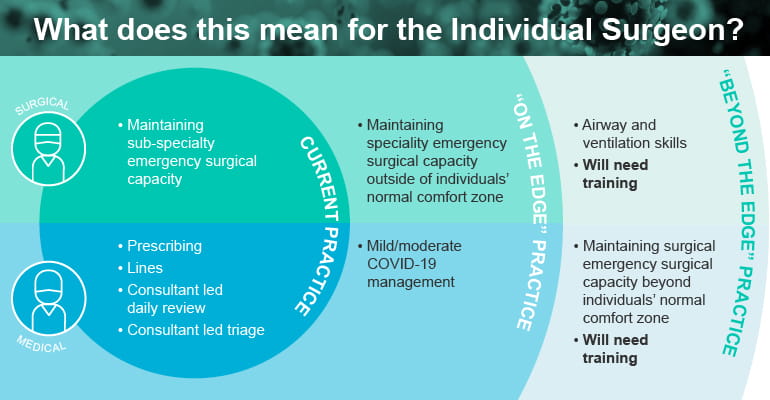
6. What does this mean for the Individual Surgeon?
6. 1 Current Practice. Medical – prescribing, lines, consultant led daily review, consultant led triage. Surgical – maintaining sub-specialty emergency surgical capacity.
6.2 “On the edge” Practice. Medical – mild/moderate COVID-19 management. Surgical – maintaining speciality emergency surgical capacity outside of individuals’ normal comfort zone.
6.3 “Beyond the edge” Practice. Medical – Airway and ventilation skills. Will need training. Surgical – Maintaining surgical emergency surgical capacity beyond individuals’ normal comfort zone. Will need training.
7. Summary
7.1 COVID-19 represents an uncertain challenge that could generate large numbers of patients in a short period of time. How best to manage this is evolving. There will not be an ideal solution so all are requested to work together to solve the challenge.
The Colleges wish to acknowledge Mr Shehan Hettiaratchy, Imperial College Healthcare NHS Trust, and Mr Dan Deakin, Nottingham University Hospitals NHS Trust, as the principal authors of this document.
